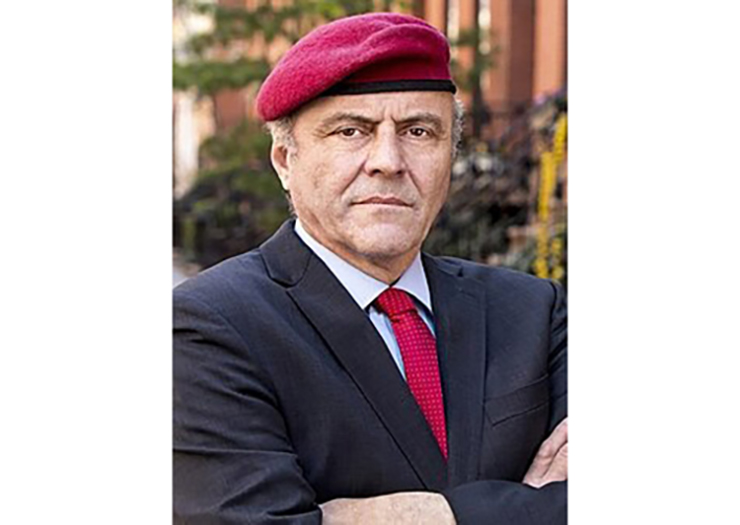
On Tuesday evening, July 13, Zicharon hosted an informative lecture with David Troxell, an internationally known expert in Alzheimer’s disease and memory care, author, and speaker.
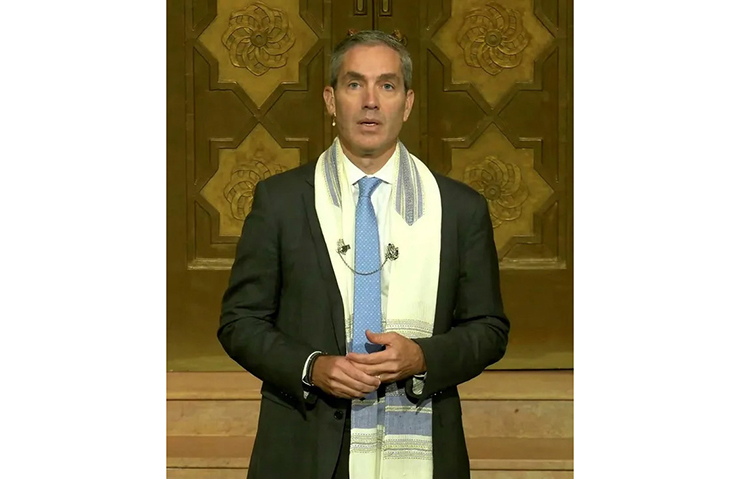
Leah Horowitz, Director of Zicharon [Zikaron, in Hebrew, means memory], shared that the goal of the program is to help us deal with the pain of dementia. Next, Sarah Cohen of the Jewish Home in Freehold, New Jersey, spoke of the unique facility that caters to people with dementia. It’s an OU-certified kosher facility with a shul and a rabbi on the premises. The atmosphere is alive and there is music and dancing and a garden. She said, “We’re here to help. And we do offer short-term respite.” She added, “You’re not in this alone. We care and know what you’re going through.”
She pointed out that dementia is a disease that is different from others. There is no cure and no set pattern. Each day is a roller coaster of behaviors. There are odd behaviors, delusions, anger, etc. The person suffering from it cannot change, because part of the brain is affected. You need the proper tool kit to avoid conflicts and to help your loved one retain her dignity.
Next, Mr. Troxell shared that there is diversity in people with Alzheimer’s. Every person is unique. It’s a blessing that we can focus on people’s strengths. He quoted the former First Lady, Rosalynn Carter: “There are four kinds of people. There are those who have been caregivers, those who are caregivers, those who will be caregivers, and those who will need a caregiver.”
Alzheimer’s is one of the most expensive diseases, and it’s the sixth leading cause of death. The difference between Alzheimer’s and dementia is that dementia is an umbrella term for confusion and memory loss, and Alzheimer’s is a type of dementia. There is no definite test for Alzheimer’s, but a doctor can diagnose one of the dementias. The number of dementias is growing.
He shared that though there is no really good drug presently, the good news is that the stigma has fallen away. One out of three families is affected by it. Research in it was woefully underfunded. Now there is up to three billion dollars invested in it.
Alzheimer’s is one of the few areas where there is bipartisanship. Years ago, it was believed you couldn’t delay the onset. However, there are things to do to delay the onset of it. A diet rich in olive oil and seafood that is heart-friendly is good. Exercise is the number one thing that helps delay it. Engagement with others helps. People who are loners succumb to it at a higher rate. Mr. Troxell shared, “The brain loves company.” He complimented the Orthodox community’s emphasis on family and community. Also, being a lifelong learner, controlling blood sugar, and getting enough sleep can also delay the onset of dementia. He said psychotropic medications are not recommended for it. He spoke about new drugs, which involve infusions once a month, and MRI scans and have significant side effects. He did not recommend them. They may help some people in early stages. His hope is that we will see better drugs in the future.
Next, he spoke about how we can support the quality of life of a person with dementia. First, keep the person as healthy as possible. They are less resilient and illness triggers dementia-related behaviors. Alzheimer’s is usually accompanied with other conditions that are treatable like pain, malnutrition, blood sugar irregularity, loneliness, and isolation. Sometimes the difficult behaviors a person is exhibiting can be related to pain. They may not be able to identify that they have pain, and they may just withdraw and grow grumpy.
Forty percent of people with dementia experience depression. A study showed that people with a long history of depression are prone to dementia. “Watch out for pain and depression.” It’s important to get financial and legal affairs in order. Don’t wait to use services. Make a game plan. Find public and private services that can help you.
He then shared the caregiver toolkit.
He listed general things that will help the person with dementia: exercise, music, art, religious and spiritual connection. He explained that the person needs a best friend with empathy and acceptance. A broken brain is invisible. We need to empathize and be more forgiving. Think of ways of how we can celebrate people’s strengths and their life stories. We have to be their biographers.
We need to learn ways to communicate, be encouraging, and be supportive. Be creative in problem-solving. “Write down their routines, preferences, achievements, as well as their professions, hobbies, favorite foods, and favorite stories that they like to share. What are their daily rituals? What is important to them? Ask them about their childhoods and ask them for life advice. Play music and offer praise. “
He emphasized that in memory care it is important to build trust and connection. Take a minute to be more person-centered. Spend time outdoors, share their favorite reading or prayers. Think about the environment. Older eyes need more light. Also make sure their environment is free of clutter.
Our brain tends to remember happy memories over sad ones, with the exception of trauma. If the person is hallucinating, be empathetic and reassuring. Be life-affirming.
Mr. Troxell added some great tips. Don’t ask too many questions, as this can add to frustration. Don’t argue or correct. You can gently cue them. In general, go with what they are saying. When things are not going well, just say, “Mom, I’m sorry. I will do better later.”
“Minimize distractions. Smile and practice positive emotional communication. They are looking for a friendly face. They are looking for a compliment. Give lots of choices as this gives them control. Ask for their opinion, as this means you value them.”
He pointed out that people with dementia say no to everything. Be proactive and try to coax them into saying yes by using different angles.
When the person keeps repeating something like a mantra, like “I want to go home,” then move them off this by asking saying something like, “Tell me about your home or your childhood,” etc.
“We need to help them feel safe, secure, and valued.” You need to realize that those suffering from dementia can be combative because they don’t understand what is going on around them. Remember that their behaviors have a root cause. Caretakers need to approach with a sense of calm and acceptance. Think of how you would act towards a friend with a migraine headache. Look for triggers or root causes. “Some people love to listen to music or to tell stories. Develop a common script.”
He also shared that siblings need to be on the same page. If a person is complaining that she doen’t want to be in assisted living, for example, develop a common script: “Mom, we know you don’t want to be here, but you need to be here to be safe or to build your strength, etc.”
He advised that the caretakers maintain a sense of optimism. “Don’t overexplain. They may have troubles processing information. Keep it simple.”
This program left the participants with a wonderful sense of optimism and, most importantly, with strategies to help them to deal with the challenges of dementia!